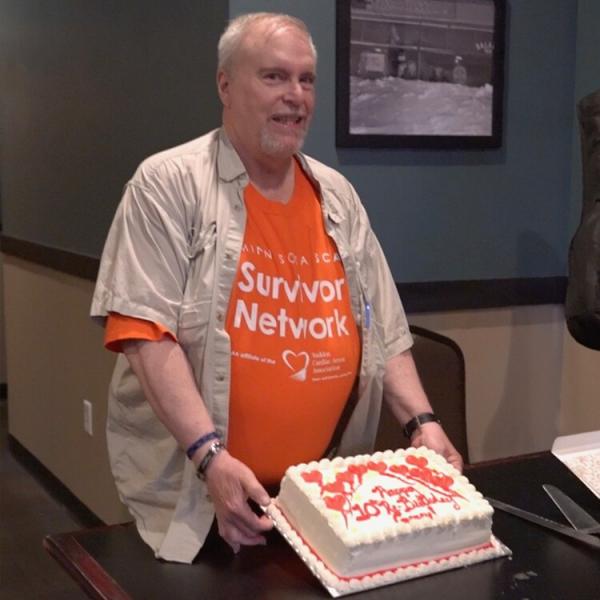
Garry's Story Canadian Photographer Celebrates His 10th ‘Re-Birthday’
Garry Frankel credits his defibrillator with peace of mind following cardiac arrest.
Garry Frankel just celebrated his 66th birthday.
But he saved the cake and the party for a celebration he considers even more important: his 10th "re-birthday."
That’s the anniversary of the day he experienced sudden cardiac arrest — when rescuers sprang into action to bring him back from the brink of death.
The then-56-year-old Canadian was sound asleep in a Minneapolis-area hotel room the night before the start of the annual USA Cup International Youth Soccer Tournament, where he volunteers his amateur photography skills. His wife, Debbie, woke up in the middle of the night after hearing Garry making strange sounds and realized he was in medical distress. She called the hotel lobby for help.
Luck was in Garry’s favor.
LUCKY BREAK
Two hotel security staff, who had just completed CPR training within the last two weeks, happened to be in the hotel lobby. They responded to the call for help within seconds, keeping Garry alive until an ambulance arrived.
During his next two weeks in the hospital, his heart stopped beating several times as a result of an arrhythmia.
“It was extremely stressful,” said Debbie. “Each time you’re wondering, ‘Is this it? What can they do to help him?’”
The answer came in the form of a Medtronic implantable cardiac defibrillator (ICD).
By the time Garry woke, the device had already been implanted and was tracking his heartbeat in order to deliver life-saving therapy and restore a normal heart rhythm if needed.
After his release from the hospital, the gravity of his condition began to sink in.
Hopefully it never will be needed, but if it’s needed it will be there, and I know my husband will have the best chance for survival having that device.
Debbie Frankel, whose husband, Garry, received ICD therapy in Minneapolis, MN
peace of mind
“I went for my first walk around the block and the thing that was always in back of my mind was, ‘If I drop while doing this, this thing is probably going to go off before I hit the ground,’” said Garry. “’And if it does, I’m probably saved. So there’s no reason for me not to go for a walk around the block,’ which then became two blocks, and three blocks and stuff like that. And now I do my whole Tai Chi set every morning.”
His wife says Garry’s device — the Evera MRI™ ICD — also gives her peace of mind.
“It was a relief to me because it meant that he does have that instant help if it’s needed,” said Debbie. “Hopefully it never will be needed, but if it’s needed it will be there, and I know my husband will have the best chance for survival having that device.”
becoming an advocate
Garry turned his medical problem into advocacy. He joined the Survivor’s Network of the Sudden Cardiac Arrest Association and used his own money to donate a portable external defibrillator (AED) to the Minnesota EMT team that helped save him.
In fact, he’s kept in touch with each person who played a role in his rescue that night 10 years ago. He even organized a special ‘10th Re-Birthday Celebration’ — complete with a re-birthday cake — so he could reconnect with his rescuers-turned-friends and thank them for their contribution to his survival.
Garry continues to volunteer his photography services year after year at the same soccer tournament that brought him to Minnesota the night his heart stopped beating. He sees it as a chance to give back to a community that helped give him an extra 10 years of life.
“If you think about it for a second, if it wasn’t for the chain of survival, if it wasn’t for the cool stuff afterward, like implantable things and all that, and if I hadn’t been coming to the tournament to take pictures, I might not be here.”
INDICATIONS, SAFETY, AND WARNINGS: EVERA MRI ICD SYSTEMS
*The Evera MRI™ SureScan™ defibrillation system is MR Conditional and, as such is designed to allow patients to be safely scanned by an MRI machine when used according to the specified MRI conditions for use. When programmed to On, the MRI SureScan feature allows the patient to be safely scanned while the device continues to provide appropriate pacing.
INDICATIONS FOR USE
The Evera MRI SureScan defibrillation system is indicated to provide ventricular antitachycardia pacing and ventricular defibrillation for automated treatment of life-threatening ventricular arrhythmias. In addition, the dual chamber devices are indicated for use in the above patients with atrial tachyarrhythmias, or those patients who are at significant risk of developing atrial tachyarrhythmias.
Notes:
- The ICD features of the device functions the same as other approved Medtronic market-released ICDs. The following notes are applicable based on the features available in the specific Evera MRI model.
- The use of the device has not been demonstrated to decrease the morbidity related to atrial tachyarrhythmias.
- The effectiveness of high-frequency burst pacing (atrial 50 Hz Burst therapy) in terminating device classified atrial tachycardia (AT) was found to be 17%, and in terminating device classified atrial fibrillation (AF) was found to be 16.8%, in the VT/AT patient population studied.
- The effectiveness of high-frequency burst pacing (atrial 50 Hz Burst therapy) in terminating device classified atrial tachycardia (AT) was found to be 11.7%, and in terminating device classified atrial fibrillation (AF) was found to be 18.2% in the AF-only patient population studied.
A complete SureScan defibrillation system is required for use in the MR environment, which is an Evera MRI SureScan ICD device with a SureScan defibrillation lead in the right ventricle and if using a dual chamber ICD, a SureScan atrial pacing lead. When a single coil SureScan defibrillation lead is used, a Medtronic DF-1 pin plug must be secured in the SVC port to make a complete SureScan DF-1 defibrillation system. To verify that components are part of a SureScan system, visit www.mrisurescan.com. Any other combination may result in a hazard to the patient during an MRI scan.
CONTRAINDICATIONS
The Evera MRI SureScan system is contraindicated for patients experiencing tachyarrhythmias with transient or reversible causes including, but not limited to, the following: acute myocardial infarction, drug intoxication, drowning, electric shock, electrolyte imbalance, hypoxia, or sepsis. The device is contraindicated for patients who have a unipolar pacemaker implanted. The device is contraindicated for patients with incessant VT or VF. For dual chamber devices, the device is contraindicated for patients whose primary disorder is chronic atrial tachyarrhythmia with no concomitant VT or VF. For single chamber devices, the device is contraindicated for patients whose primary disorder is atrial tachyarrhythmia.
WARNINGS AND PRECAUTIONS
Changes in patient’s disease and/or medications may alter the efficacy of the device’s programmed parameters. Patients should avoid sources of magnetic and electromagnetic radiation to avoid possible underdetection, inappropriate sensing and/or therapy delivery, tissue damage, induction of an arrhythmia, device electrical reset, or device damage. Do not place transthoracic defibrillation paddles directly over the device.
Patients and their implanted systems must be screened to meet the following requirements for MRI: no implanted lead extenders, lead adaptors, or abandoned leads; no broken leads or leads with intermittent electrical contact as confirmed by lead impedance history; a SureScan defibrillation system implanted in the left or right pectoral region; pacing capture thresholds of ≤ 2.0 V at a pulse width of 0.4 ms; no diaphragmatic stimulation at a pacing output of 5.0 V and at a pulse width of 1.0 ms in patients whose device will be programmed to an asynchronous pacing mode when MRI SureScan is programmed to On.
Patients may be scanned using a horizontal field, cylindrical bore, clinical 1.5T or 3T MRI system for hydrogen proton imaging, maximum spatial gradient ≤ 20 T/m, and maximum gradient slew rate performance per axis ≤ 200 T/m/s. 1.5T scanners must be operated in Normal Operating Mode (whole body averaged specific absorption rate (SAR) ≤ 2.0 W/kg, head SAR ≤ 3.2 W/kg). 3T scanners must be operated in First Level Controlled Operating Mode or Normal Operating Mode. B1+RMS must be ≤ 2.8 μT when the isocenter (center of the bore) is inferior to the C7 vertebra. Scans can be performed without B1+RMS restriction when the isocenter is at or superior to the C7 vertebra.
Continuous patient monitoring is required while MRI SureScan is programmed to On. While MRI SureScan is programmed to On, arrhythmia detection and therapies are suspended, leaving the patient at risk of death from untreated spontaneous tachyarrhythmia. In addition, if the device is programmed to an asynchronous pacing mode, arrhythmia risk may be increased.
POTENTIAL COMPLICATIONS
Potential complications include, but are not limited to, rejection phenomena, erosion through the skin, muscle or nerve stimulation, oversensing, failure to detect and/or terminate tachyarrhythmia episodes, acceleration of ventricular tachycardia, and surgical complications such as hematoma, infection, inflammation, and thrombosis. Other potential complications related to the lead may include lead dislodgement, lead conductor fracture, insulation failure, threshold elevation, or exit block.
The SureScan system has been designed to minimize potential complications in the MRI environment. Potential MRI complications include, but are not limited to, lead electrode heating and tissue damage resulting in loss of sensing or capture or both, or MR-induced stimulation on leads resulting in continuous capture, VT/VF, and/or hemodynamic collapse.
See the MRI SureScan Technical Manual before performing an MRI Scan and Device Manual for detailed information regarding the implant procedure, indications, contraindications, warnings, precautions, and potential complications/adverse events. For further information, please call Medtronic at 1-800-328-2518 and/or consult the Medtronic website at medtronic.com or mrisurescan.com.
Caution: Federal law (USA) restricts this device to sale by or on the order of a physician.