Harnessing Extended Reality To Revolutionize Healthcare
Researchers are experimenting with extended reality (XR) technology in every division of Medtronic.
From the moment he put on the headgear, Vanderbilt University electrophysiologist Dr. George Crossley could see the possibilities.
“It took about 10 seconds of having this tool on my head to show me the power of having a physician see what's happening inside the heart,” he said.
Dr. Crossley was practicing implants of Micra™ — the world’s smallest pacemaker — using an experimental, 3-D simulator that incorporates extended reality (XR) technology.
The XR feature, using the Microsoft HoloLens and software developed by CAE Healthcare, allowed him to navigate inside a virtual, beating heart.
The simulation was so realistic, Crossley was convinced it could revolutionize the training of cardiologists.
“It lets us get the trainee to a much higher level, using a simulator, than we could in a hundred cases with a live patient,” he said.
The Micra™ simulator is just one of 80 XR technology projects currently underway at Medtronic.
It lets us get the trainee to a much higher level.
Dr. George Crossley on the benefits of using XR technology in surgical training simulations.
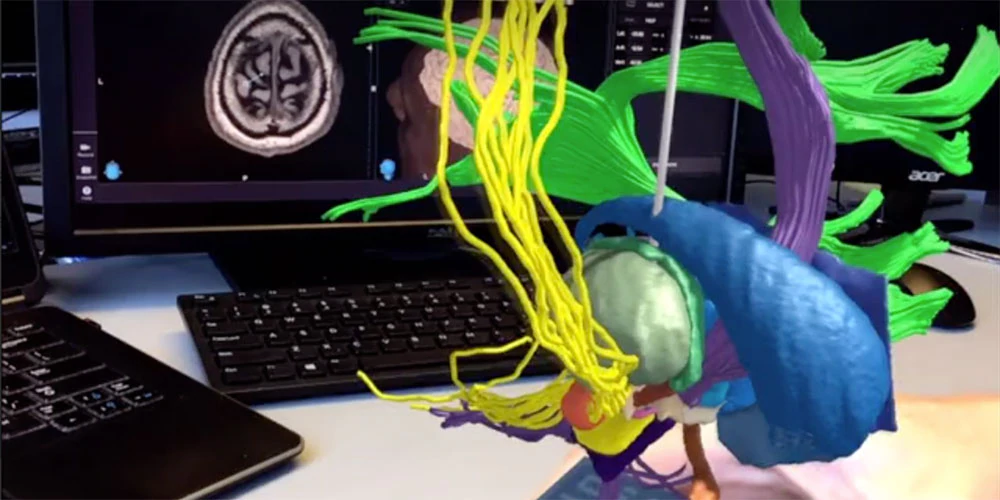
The work includes Virtual Reality, which is a completely computer-generated experience, and Augmented Reality (AR), which overlays virtual elements over a real environment. Extended Reality (XR) refers to a combination of all real and virtual environments generated by technology and wearables.
Medtronic experts agree the potential for XR technology to revolutionize healthcare extends far beyond cardiology.
Medtronic Diabetes already uses holograms to help educate patients about diabetes therapy or to troubleshoot their insulin pumps. And they’re developing XR programs to help train on the best way to insert glucose sensors.
“Ultimately, our goal is that patients have to think less about their Diabetes,” said Rebecca Gottlieb, Ph.D., Vice President of Research and Technology at Medtronic Diabetes. “For me, the future isn't scary, it's really exciting.”
POTENTIAL IMPACT ON HEALTHCARE COSTS AND EVERYDAY LIFE
Studies have shown1 that many of the 425 million people2 worldwide who live with diabetes struggle to control their disease, and that struggle is costly. It’s estimated that every year, nearly 300,000 people with diabetes visit an emergency room in the U.S. for hypoglycemia, and about 175,000 go to an ER for hyperglycemic crises.3 Helping people with diabetes manage their diet has the potential to save health systems money by reducing the need for medical intervention.
Gottlieb and her teams are exploring several XR technology-related ideas that could help people living with diabetes manage their daily diets.
“Let’s say you walk into a restaurant,” Gottlieb said. “You look at the menu. Smart glasses could read the menu and maybe we highlight for you what the best choice is based on your current glucose reading.”
People with diabetes often need to be experts in tracking and counting carbohydrates. But some day, a smart device might count the carbs on their plate, and predict how their bodies will respond. ”Diabetes is a disease of data,” Gottlieb said. “Patients are constantly having to think and adjust. ‘Am I stressed? Am I feeling okay? Am I about to exercise? Should I eat something?’ All of those calculations have to spin around in their heads all day. What we're hoping to do is give them that brain space back so they can go on with their lives.”
TECHNOLOGY FRONTIER: WHAT LIES AHEAD
Researchers are experimenting with XR technology in every division of Medtronic.
Jay Reid is a director of heart procedure training. He sees similarities between this research and space exploration of the 1960s and 1970s.
'I think it is a big deal, and I think the sky is the limit,” Reid said. “In the medical device world, we are on that leading edge, exploring space — virtual and digital space — that we have thought about, dreamed about. Now it's coming to fruition.”
One such concept involves importing MRI or CT scans of a patient into an extended reality simulator, allowing doctors to practice a surgical procedure on a virtual replica of a person’s anatomy before performing the actual surgery.
FAST FACT: MORE THAN 80 EXTENDED REALITY PROJECTS ARE NOW UNDERWAY AT MEDTRONIC, IN EVERY DIVISION OF THE COMPANY.
“What might seem futuristic is really here today. It's what's happening now,” said Brian Bechard, a member of the Medtronic Healthcare Innovation Team within the company's Digital Health, Emerging Technologies group. “The XR technology projects currently in progress allow us to put our hands around what this space can become. I’m really excited about what the next five years hold for us.”
Bechard believes it’s only a matter of time before XR technology is used during a live surgical procedure. And he envisions a day when the combination of XR, robotics and artificial intelligence might allow a surgeon to operate on a patient located miles away.
Wherever the technology leads, doctors like Crossley are encouraged about the possibilities of turning “extended reality” into an “actual reality” that improves the lives of patients.
"If I close my eyes and think about what the future could look like, that's a very nice picture,” Crossley said.
REFERENCES
1 http://care.diabetesjournals.org/content/36/5/13842 https://www.idf.org/aboutdiabetes/what-is-diabetes/facts-figures.html
3 http://clinical.diabetesjournals.org/content/diaclin/early/2017/12/20/cd17-0094.full.pdf
IMPORTANT INFORMATION
Diabetes-related technology discussed in this story is future technology that is not available commercially and that has not been approved by the Food and Drug Administration (FDA).
IMPORTANT SAFETY INFORMATION: MICRA TRANSCATHETER PACING SYSTEM VVIR SINGLE CHAMBER WITH SURESCAN™ MRI
Indications
Micra Model MC1VR01 is indicated for patients with:
- symptomatic paroxysmal or permanent high-grade AV block in the presence of AF,
- symptomatic paroxysmal or permanent high-grade AV block in the absence of AF, as an alternative to dual chamber pacing when atrial lead placement is considered difficult, high risk, or not deemed necessary for effective therapy,
- symptomatic bradycardia-tachycardia syndrome or sinus node dysfunction (sinus bradycardia/sinus pauses), as an alternative to atrial or dual chamber pacing when atrial lead placement is considered difficult, high risk, or not deemed necessary for effective therapy.
Rate-responsive pacing is indicated to provide increased heart rate appropriate to increasing levels of activity.
Contraindications
Micra model MC1VR01 is contraindicated for patients who have the following types of medical devices implanted: an implanted device that would interfere with the implant of the Micra device in the judgment of the implanting physician, an implanted inferior vena cava filter, a mechanical tricuspid valve, or an implanted cardiac device providing active cardiac therapy that may interfere with the sensing performance of the Micra device.
The use of deactivated Micra devices in situ and an active Micra device, or an active transvenous pacemaker or defibrillator, has not been clinically tested to determine whether EMI or physical interaction is clinically significant. Bench testing supports that implantation of an active Micra device, or an active transvenous pacemaker or defibrillator, next to an inactivated Micra device is unlikely to cause EMI or physical interaction. post-approval studies are planned to characterize risks of co-implanted, deactivated Micra devices. Currently recommended end of device life care for a Micra device may include the addition of a replacement device with or without explantation of the Micra device, which should be turned off.
Contraindications
The device is contraindicated for patients who have the following conditions: femoral venous anatomy unable to accommodate a 7.8 mm (23 French) introducer sheath or implant on the right side of the heart (for example, due to obstructions or severe tortuosity), morbid obesity that prevents the implanted device from obtaining telemetry communication within ≤12.5 cm (4.9 in), or known intolerance to the materials listed in the Instruction for Use, or to heparin, or sensitivity to contrast media that cannot be adequately premedicated, or where a single dose of 1.0 mg dexamethasone acetate may be contraindicated.
Precautions should be taken before administering anticoagulant agents, antiplatelet agents, or contrast media in patients with known hypersensitivity to these agents.
The following may be contraindications to Micra VVIR pacing. Rate-responsive mode may be contraindicated for patients who cannot tolerate pacing rates above the programmed Lower Rate. Asynchronous VVIR pacing with sinus rhythm may be contraindicated when competitive pacing is considered undesirable or causes symptoms of pacemaker syndrome. The patient’s age and medical condition should be considered by physicians and patients as they select the pacing system, mode of operation, and implant technique best suited to the individual.
Warnings and Precautions
End of Service (EOS) – When the EOS condition is met, the clinician has the option of permanently programming the device to Off and leaving it in the heart, or retrieving the device, provided the device has not yet become encapsulated. Removal of the Micra device after it has become encapsulated may be difficult because of the development of fibrotic tissue. If removal of the device is required, it is recommended that the removal be performed by a clinician who has expertise in the removal of implanted leads.
MRI conditions for use – Before an MRI scan is performed on a patient implanted with the Micra device, the cardiology and radiology professionals involved in this procedure must understand the requirements specific to their tasks as defined in the device manuals.
Potential Complications
Potential complications include, but are not limited to, toxic/allergic reaction, oversensing, acceleration of tachycardia, myocardial infarction and surgical complications such as cardiac perforation, pericardial effusion, cardiac tamponade, death, device embolization, access site hematoma and AV fistulae, vessel spasm, infection, inflammation, and thrombosis.
See the device manuals for detailed information regarding the implant procedure, indications, contraindications, warnings, precautions, MRI conditions for use, and potential complications/adverse events. For further information, please call Medtronic at 1-800-328-2518 and/or consult Medtronic’s website at www.medtronic.com.
Caution: Federal law (USA) restricts these devices to sale by or on the order of a physician.
L001-01232019