World’s Smallest Pacemaker Passes Space Test
Micra™ TPS remains functioning after bumpy rocket ride into space.
The world’s smallest pacemaker aced its space test.
Medtronic’s Micra™ Transcatheter Pacing System (TPS) not only survived a bumpy, 13-minute, 73-mile-high rocket ride into Earth’s sub-orbit, but initial interrogation of the device done a few hours after launch showed the device still functioning the way engineers had designed.
“Just fantastic news,” said senior program manager Wade Demmer, who spent eight years working on Micra TPS for Medtronic.
Micra TPS was among dozens of experiments packed into the nose cone of NASA’s 36-foot long, Terrier-Improved Orion sounding rocket. .
>
'In some ways this is well beyond what they'd ever send an astronaut into.'
Wade Demmer, senior program manager, Medtronic
The June 22 launch subjected the device to more than 20 times the force of gravity, vibrations “worse than a paint shaker,” temperatures reaching 140 degrees Fahrenheit, radiation from Earth’s sub-orbit and a splashdown in the Atlantic Ocean.
“This isn’t a manned rocket. It doesn’t come with the protections that an astronaut gets,” Demmer said.
“In some ways this is well beyond what they’d ever send an astronaut into. So to know that Micra was still operating properly after all that is a really good feeling.”
'I think there's going to be a lot of damage, but I could be wrong.'
Shelbi Klingsporn
High School Science Project
The idea to launch and test Micra in space came from 17-year-old Shelbi Klingsporn, a high school student from Scottsbluff, Nebraska.
Encouraged by science teacher Katie Juarez and English teacher Lesley Billingsley, Shelbi submitted a proposal, complete with diagrams and a written summary, to the Cubes in Space (CIS) project. Cubes in Space is a private, non-profit education program that, in partnership with NASA, encourages students to get involved in science and space. Hundreds of students from around the world submitted ideas – Shelbi’s was among just 80 selected for the flight. Learn more.
Students picked for Cubes in Space were invited to NASA’s Wallops Flight Facility near Chincoteague, Virginia, to watch the launch. They also set up exhibits in NASA’s Visitor Center on the day before liftoff and explained their experiments to the general public. Shelbi’s presentation included a hypothesis that the Micra TPS, which contains some glass components and wires thinner than a human hair, could not withstand the brutal G-forces of the launch.
“Personally I don’t think it’s going to come back and operate or function like we want,” she said as she watched the rocket race into space. “I think there’s going to be a lot of internal damage. But I could be wrong. You never know.”
Preparing for Launch
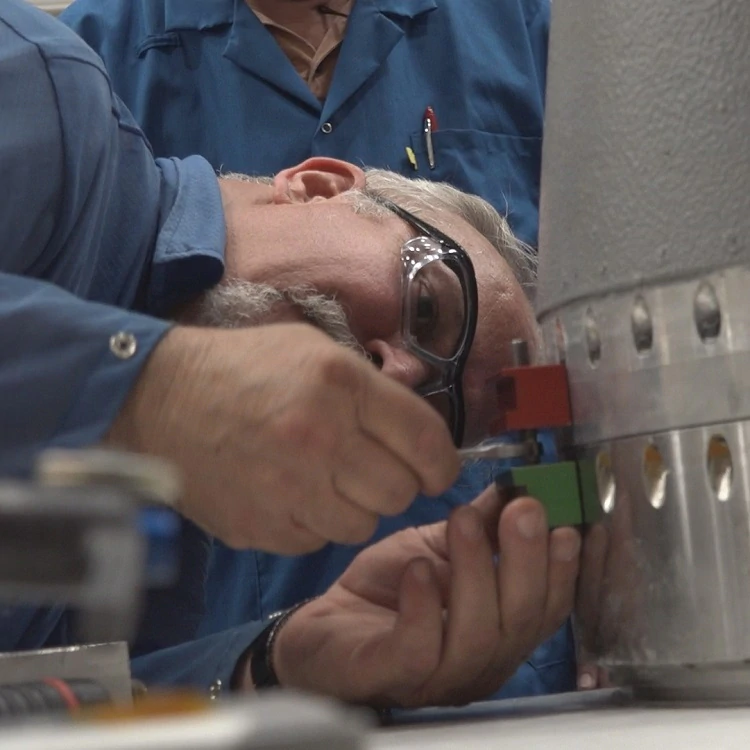
Demmer and Tom Anderson, another Medtronic engineer who helped develop Micra TPS, shared her concern. After Shelbi contacted Medtronic with her idea, Demmer and Anderson gave her advice and support. Medtronic provided a working device for the flight, and Anderson added a resistor to mimic the electrical activity inside a human body. “So the Micra TPS would think it was pacing a real person,” Demmer said.
The two engineers attended the launch with Shelbi and her teachers, and brought along special equipment to interrogate the Micra device as soon as it returned from space.
Eight hours after launch, and two hours after the payload returned to NASA’s hanger, they got their answer.
Post-Flight Interrogation and Examination
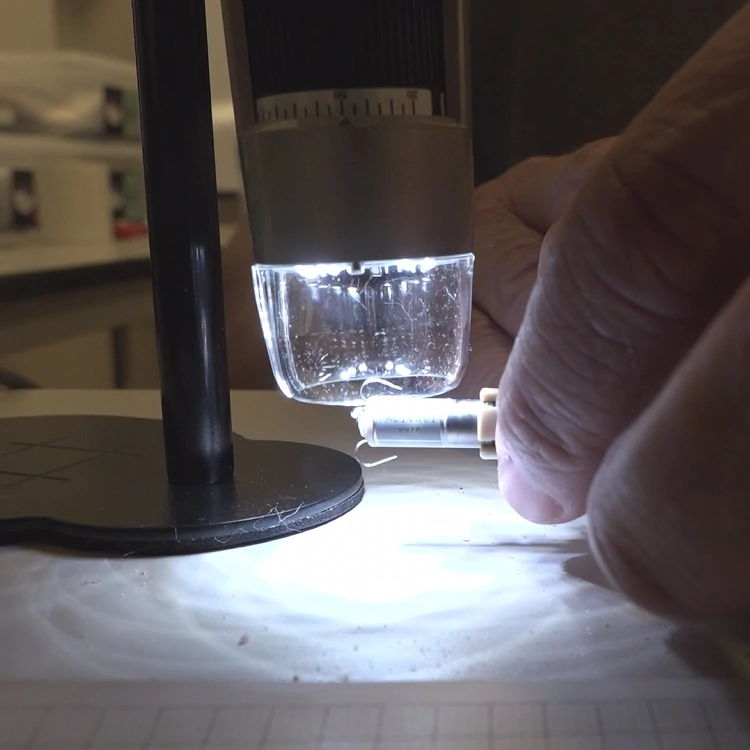
Using a special computer programmer, Demmer “interrogated” Micra TPS by hovering a reader over the device – his computer screen sprang to life as Micra immediately “answered.”
“Just for that little thing to happen the battery had to work, the circuit had to work, and the antennae had to work, and those were the three major components that we worried about,” Demmer said.
The interrogator downloaded data from the device. That information showed Micra TPS, which is designed to automatically adjust pacing therapy based on a person’s activity levels, had increased its pacing rate during the flight, and lowered it again afterward. “Micra interpreted the shaking as exercise and increased its pacing, which is what it’s supposed to do,” Demmer said. “That means the accelerometer inside the device is also working. Great news.”
What's Next
Shelbi will turn 18 during the summer and wants to become a physician’s assistant. “I’ve learned a lot about pacemakers and the field of medicine,” she said. “And I learned about how to conduct good research. Every part of this experience really helped.”
Medtronic may do more testing on the device, and students with other experiments on board are planning to share information with Demmer and Anderson about radiation levels and other data their projects gathered during the flight.
“This test doesn’t mean that anyone with a pacemaker can go into space,” Demmer said. “But the idea that someone with a medical device, might someday be able to travel into space isn’t as far-fetched today as it was yesterday.”
Note: Patients are encouraged to consult with their physician regarding their lifestyle and activities while implanted with the Micra TPS.
June 30, 2017
Micra Transcatheter Pacing System
Additional Device Information
An implantable pacemaker system relieves symptoms of heart rhythm disturbances. They do this by restoring normal heart rates. A normal heart rate provides your body with the proper amount of blood circulation. The pacemaker system is intended for patients who need rate-adaptive pacing or chronic pacing.
Risks associated with the Micra Transcatheter Pacing System (Micra) implant include, but are not limited to, complications at the surgical site, injury to the heart where the device is attached such as pericardial effusion (fluid around the heart) and/or sensitivity to the device material, failure to deliver therapy when it is needed, or receiving extra therapy when it is not needed. After receiving a Micra, you will have limitations with certain magnetic and electromagnetic radiation, electric or gas powered appliances and tools in which you are allowed to be in contact.
Once implanted, removal of the Micra after it has become encapsulated may be difficult because of the development of fibrotic tissue. At such time, your physician has the option of permanently turning off the Micra, and leaving it in the heart.
This treatment is prescribed by your physician. This treatment is not for everyone. Please talk to your doctor to see if it is right for you. Your physician should discuss all potential benefits and risks with you. Although many patients benefit from the use of this treatment, results may vary. For further information, please call the Medtronic toll-free number at 1-800-551-5544 (7:00 a.m. to 6:00 p.m., Monday–Friday, Central Time) or see the Medtronic website at www.medtronic.com.
Important Safety Information: Micra Transcatheter Pacing System VVIR Single Chamber with SureScantm MRI
INDICATIONS
Micra Model MC1VR01 is indicated for patients with:
- symptomatic paroxysmal or permanent high grade AV block in the presence of AF,
- symptomatic paroxysmal or permanent high grade AV block in the absence of AF, as an alternative to dual chamber pacing when atrial lead placement is considered difficult, high risk, or not deemed necessary for effective therapy,
- symptomatic bradycardia-tachycardia syndrome or sinus node dysfunction (sinus bradycardia/sinus pauses), as an alternative to atrial or dual chamber pacing when atrial lead placement is considered difficult, high risk, or not deemed necessary for effective therapy.
Rate-responsive pacing is indicated to provide increased heart rate appropriate to increasing levels of activity.
CONTRAINDICATIONS
Micra Model MC1VR01 is contraindicated for patients who have the following types of medical devices implanted: an implanted device that would interfere with the implant of the Micra device in the judgment of the implanting physician, an implanted inferior vena cava filter, a mechanical tricuspid valve, or an implanted cardiac device providing active cardiac therapy that may interfere with the sensing performance of the Micra device.
The device is contraindicated for patients who have the following conditions:femoral venous anatomy unable to accommodate a 7.8 mm (23 French) introducer sheath or implant on the right side of the heart (for example, due to obstructions or severe tortuosity), morbid obesity that prevents the implanted device from obtaining telemetry communication within ≤12.5 cm (4.9 in), or known intolerance to the materials listed in the Instruction for Use, or to heparin, or sensitivity to contrast media that cannot be adequately premedicated.
Steroid use – Do not use in patients for whom a single dose of 1.0 mg of dexamethasone acetate cannot be tolerated.
WARNINGS AND PRECAUTIONS
End of Service (EOS) – When the EOS condition is met, the clinician has the option of permanently programming the device to Off and leaving it in the heart, or retrieving the device, provided the device has not yet become encapsulated. Removal of the Micra device after it has become encapsulated may be difficult because of the development of fibrotic tissue. If removal of the device is required, it is recommended that the removal be performed by a clinician who has expertise in the removal of implanted leads.
MRI conditions for use – Before an MRI scan is performed on a patient implanted with the Micra device, the cardiology and radiology professionals involved in this procedure must understand the requirements specific to their tasks as defined in the device manuals.
Rate-responsive mode may not be appropriate for patients who cannot tolerate pacing rates above the programmed Lower Rate. Asynchronous VVIR pacing with sinus rhythm may not be appropriate when competitive pacing is considered undesirable or causes symptoms of pacemaker syndrome. The patient’s age and medical condition should be considered by physicians and patients as they select the pacing system, mode of operation, and implant technique best suited to the individual.
Precautions should be taken before administering anticoagulant agents, antiplatelet agents, or contrast media in patients with known hypersensitivity to these agents.
The use of deactivated Micra devices in situ and an active Micra device, or an active transvenous pacemaker or defibrillator, has not been clinically tested to determine whether EMI or physical interaction is clinically significant. Bench testing supports that implantation of an active Micra device, or an active transvenous pacemaker or defibrillator, next to an inactivated Micra device is unlikely to cause EMI or physical interaction. Post-approval studies are planned to characterize risks of co-implanted, deactivated Micra devices. Currently recommended end of device life care for a Micra device may include the addition of a replacement device with or without explantation of the Micra device, which should be turned off.
POTENTIAL COMPLICATIONS
Potential complications include, but are not limited to, toxic/allergic reaction, oversensing, acceleration of tachycardia, myocardial infarction and surgical complications such as cardiac perforation, pericardial effusion, cardiac tamponade, death, device embolization, access site hematoma and AV fistulae, vessel spasm, infection, inflammation, and thrombosis.
See the device manuals for detailed information regarding the implant procedure, indications, contraindications, warnings, precautions, MRI conditions for use, and potential complications/adverse events. For further information, please call Medtronic at 1-800-328-2518 and/or consult Medtronic’s website at www.medtronic.com.
Caution: Federal law (USA) restricts these devices to sale by or on the order of a physician.