Changing the standard of care for stroke
Medtronic device helps reduce disability associated with stroke.
At 42, Stefan Reisch was active, fit and lived to surf. The last person you’d expect to have health problems.
“I was driving to work, I had a bruise on my neck,” he recalls. “I rubbed it, and about five seconds later I felt like I was going to pass out. And I proceeded to have a stroke.”
A stroke. In the middle of a San Diego morning rush hour, a blood clot lodged in Stefan’s brain – blinding his left eye and paralyzing his left side. Stefan’s car came to a crashing halt.
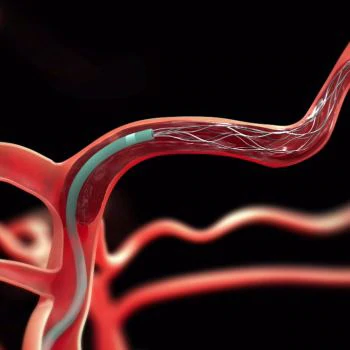
The EMT on the scene identified the signs of stroke and directed the ambulance to take Stefan to a certified stroke center. There he was given IV drug treatment, and then a neurosurgeon inserted a Medtronic device called “Solitaire” into an artery in Stefan’s groin. They guided it into his brain and retrieved the clot that was obstructing proper blood flow.
“We saw the immediate result in terms of restoration of movement on the left side of his body,” said neurosurgeon Alexander A. Khalessi, MD, Vice-Chairman of Clinical Affairs at the University of California San Diego Health System, who performed the procedure. “And I can tell you it’s a very rare and special privilege to have that experience and be able to share that with the patient,” he said.
Stefan left the hospital within days of the procedure. He returned to work in just two weeks.
His recovery represents a potential milestone in healthcare.
Historically, stroke is a leading cause of disability worldwide2. In the US alone, stroke costs 74 billion dollars a year in hospital bills, rehab and long term care of disabled stroke victims.3
But now, Medtronic Neurovascular studies confirm that in stroke cases like Stefan’s, use of Solitaire plus clot-busting drugs, can nearly double a stroke victim’s chances of returning to a functional life. And can cut the average hospital time from a couple of months (73 days) to a couple of weeks (15 days).4
Such improved patient outcomes have the potential to save healthcare systems billions of dollars every year.
Medical results have been so impressive - the American Heart Association/American Stroke Association revised its standard of care guidelines last year to recommend using devices like Solitaire in cases like Stefan’s.
Fifteen million people suffer acute ischemic strokes each year worldwide2 (695,000 in the United States). It’s believed the Solitaire device could help almost five million of them (240,000 in the United States), but in 2014 only 40,000 patients received therapy using the Solitaire device (13,000 in the United States). It’s currently available at an estimated 500 hospitals in the United States.5
LEARN MORE
Read the Medtronic Perspective on Transforming Healthcare:
Transforming Medtronic to Support Progress in Healthcare (PDF)(opens new window)
Important Safety Information
INDICATIONS FOR USE
The Solitaire™ 2 Revascularization Device is indicated for use to restore blood flow in the neurovasculature by removing thrombus for the treatment of acute ischemic stroke to reduce disability in patients with a persistent, proximal anterior circulation, large vessel occlusion, and smaller core infarcts who have first received intravenous tissue plasminogen activator (IV t-PA). Endovascular therapy with the device should be started within 6 hours of symptom onset.
Possible Complications
- Possible complications from the use of this device include, but are not limited to:
- Bruising and bleeding at the puncture site
- Blockage, puncturing, tearing or spasms of the blood vessel
- Blood clot formation outside the artery
- Post procedure bleeding
- Change in mental status
- Neurologic deterioration including stroke and death
- Infection
- Adverse reaction to blood thinners or contrast media
- Deformation, collapse, fracture or malfunction of the device
- Bleeding within the skull
- Interruption of blood flow to the heart or other organs
- Blood clotting or air bubbles within the circulatory system
- Formation of an abnormal connection between an artery and a vein
- Distal embolization including to a previously uninvolved territory
References
1 Kochanek KD, Murphy SL, Xu JQ, Arias E. Mortality in the United States, 2013. NCHS data brief, no 178. Hyattsville, MD: National Center for Health Statistics. 2014.
2 World Heart Federation Stroke Statistics, http://www.world-heart-federation.org/cardiovascular-health/stroke/
3 Guzauskas, Gregory F., The Cost-Effectiveness of Primary Stroke Centers for Acute Stroke Care, Stroke. 2012;43:1617-1623; originally published online 25 April 2012
4 Campbell, Bruce C. New England Journal of Medicine. Endovascular Therapy for Ischemic Stroke with Perfusion-Imaging Selection, 11 Feb. 2015; Goyal Mayank. New England Journal of Medicine. Randomized Assessment of Rapid Endovascular Treatment of Ischemic Stroke, 11 Feb. 2015.
5 Press Release, American Heart Association's New Stroke Treatment Guidelines Establish Stent Retrievers as First-Line Endovascular Treatment for Acute Ischemic Stroke, 29 June 2015